| Neuropathic Pain |
| Neuropathic pain can occur with traumatic peripheral nerve injury due to an accident, surgery, or entrapment (eg, carpal tunnel syndrome) or following nerve root (eg, radiculopathy) or spinal nerve injury.Some other conditions associated with neuropathic pain include diabetic neuropathy, postherpetic neuralgia (PHN), complex regional pain syndrome, phantom limb pain, and trigeminal neuralgia.One Finnish study found that more than 8% of people with newly diagnosed type 2 diabetes already had evidence of DPN and that almost 42% of people with diabetes had DPN 10 years after diagnosis.Approximately 10% to 15% of people with herpes zoster develop PHN; although the incidence of neuropathic pain with herpes zoster is almost 50% in people older than 60 years of age.
There are 2 types of complex regional pain syndromes: type I (formerly called reflex sympathetic dystrophy; RSD) does not involve an obvious injury to the nervous system and it is debatable whether this is a true neruopathic pain syndrome. Complex regional pain syndrome type II, formerly referred to as causalgia, follows an injury to a nerve. It may occur as the result of surgery involving a nerve, such as a carpal tunnel release. References: Galer BS, Dworkin RH. A Clinical Guide to Neuropathic Pain. Minneapolis, Minn: Healthcare Information Programs; 2000:120-123. Partanen J, Niskanen L, Lehtinen J, et al. Natural history of peripheral neuropathy in patients with non-insulin- dependent diabetes mellitus. N Engl J Med. 1995;333:89-94. Rowbotham M, Harden N, Stacey B, et al, for the Gabapentin Postherpetic Neuralgia Study Group. Gabapentin for the treatment of postherpetic neuralgia. A randomized controlled trial. JAMA. 1998;280:1837-1842. Serra J. Overview of neuropathic pain syndromes. Acta Neurol Scand.1999:173:7-11.
2) Prevalence of Neuropathic Pain The prevalence of neuropathic pain in the UK is approximately 1% of the population, similar to the 0.6% to 1.5% estimate of prevalence in the United States. Conservative estimates of prevalence in 1998 suggest diabetic polyneuropathy (DPN) case numbers of 94,000 (France), 242,000 (Germany), 114,000 (Italy), 50,000 (Spain), 116,000 (UK), and 251,000 (Japan). PHN is less prevalent: 71,000 (France), 108,000 (Germany), 79,000 (Italy), 49,000 (Spain), 75,000 (UK), and 163,000 (Japan). Trigeminal neuralgia cases are similar across major European countries (prevalences 11,000 to 27,000). Previous estimates have assumed that 1 in 10 cases of lower back pain have a neuropathic pain component, which suggests an estimated prevalence of more than 1.2 million cases of neuropathic back pain in Europe and Japan. These figures suggest that there is a similar prevalence of neuropathic pain among developed countries. In many cases, the non-pain specialist will be the first healthcare provider to manage the patient with neuropathic pain. Therefore, it is necessary to understand what neuropathic pain is, the underlying mechanisms that lead to neuropathic pain, and strategies for managing pain and improving patient quality of life. 3) The Neuropathic Pain Challenge
4) Development of Neuropathic Pain The key talking points on this are as follows:
Studies are needed to further define pathophysiological mechanisms of neuropathic pain. 5) Diagnosis a) In conclusion, the evaluation of the patient suspected of having neuropathic pain requires an assessment of the total patient. b) Neuropathic pain might be suspected in patients who present with no apparent reason for their pain. c) A pain history must be obtained, including a full description of the patient’s symptoms and the intensity of pain as measured by pain scales, as well as an assessment of underlying causes. The latter can be determined by a thorough medical review of systems, surgical history, and physical examination. d) Simple bedside tests can aid the clinician greatly in identifying the patient with neuropathic pain. If necessary, diagnostic studies such as EMG or NCS may be ordered by the non-pain specialist to more fully categorize areas of involvement. However, it is important to remember that the results of these diagnostic tests may be normal in the presence of neuropathic pain. Thus, the clinician must work from the symptoms toward the diagnosis. e) It is also important to remember that many patients with neuropathic pain suffer from comorbid conditions, which can confound both diagnosis and treatment. 6) Physical Abnormalities in the Painful Area
a) Inspect the painful body area and compare it with the corresponding healthy area :
b) Conduct simple bedside tests to confirm sensory abnormalities associated with pain symptoms :
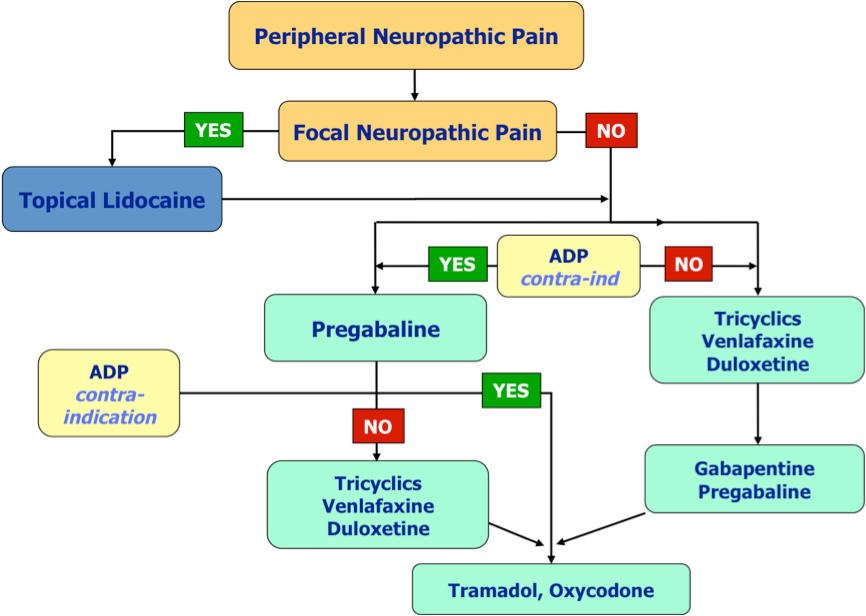
7) Goals of Neuropathic Pain Treatment Primary goal = reduction in pain Secondary goals
8) Quick Assesment If yes for the any above, please contact us for a consultation. |